Getting enough good quality sleep is important for maintaining normal blood sugar levels and reducing insulin resistance. According to the Centers for Disease Control and Prevention (CDC), adults should be getting somewhere between seven and nine hours of sleep per night. Many of us do not do this, the effect is the disruption of normal metabolic processes such as blood sugar regulation.
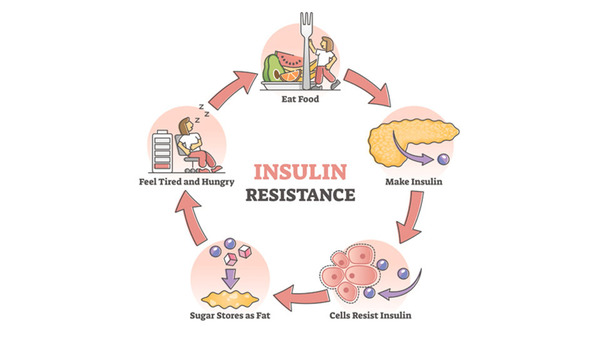
Insulin is a hormone secreted by the pancreas that allows cells throughout the bod to take glucose (sugar) from blood and use it for energy. Glucose is found throughout the body, especially in muscle, fat and liver cells. After a meal, blood sugar levels rise, and insulin is released to bring blood sugar levels down. Normal blood levels are defined as 70 – 100 mg/dL when fasting and less than 140 mg/dL two hours after a meal.
The body rests between meals as well as during sleep, allowing insulin levels to fall, allowing blood sugars to be maintained by glucose release from liver cells. This rest cycle keeps blood sugars in the normal range. Insufficient sleep can disrupt the process negatively in several ways.
- Not getting enough sleep triggers higher baseline insulin levels, indicating increased insulin resistance. Higher insulin levels are needed to maintain normal blood sugar levels.
- A reduction in sleep increases post-meal blood sugar spikes. Blood sugars rise higher and stay elevated longer after meals.
- Insufficient sleep adversely affects the pancreas. The pancreas secretes less insulin following blood sugar spikes when sleep deprived.
- Insufficient sleep is linked to a reduced glucose tolerance, which increases the risk of diabetes.
- Sleep deprivation leads to the munchies! Reduced sleep alters one’s appetites, leading to more calories consume, weight gain, and a higher body fat percentage.
Lab tests for monitoring insulin resistance
There are several lab tests to help monitor us for insulin resistance and possible diabetes risk:
A fasting plasma glucose test measures blood sugar after more than 8 hours without food. A level of 126 mg/dL or higher indicates diabetes. An oral glucose tolerance test measures blood sugar before and 2 hours after a high glucose drink. It is used to diagnose prediabetes and diabetes. And lastly, a hemoglobin A1C test can be used. It estimates average blood sugar over 2-3 months. Ranges for pre-diabetes are 5.7 – 6.4%, while diabetes is 6.5% or more.
A primary oral first line medication is metformin. While it decreases glucose production in the liver, it also assists with cardiovascular health. According to the NIH, “Type 2 diabetes mellitus (T2DM) is a world-wide major health burden and heart failure (HF) is the most common cardiovascular (CV) complication in affected patients.
Sometimes the pancreas doesn’t respond to oral medications, whether it be metformin, or any other medications. There are several types of injectable insulin that can be used in diabetes treatment. They are categorized by their duration of action. Rapid-acting insulin starts working in 15 minutes, and peaks in 60-90 minutes. Insulins such as Novolog and Humalog fall into this category. Short-acting insulin starts working in 30-60 minutes, peaks in 2-3 hours and stays active in the body for 3 – 6 hours. Intermediate-acting insulin takes 2 – 4 hours to start working. It peaks in 4 – 10 hours, and works for up to 18 hours. Long-acting insulin stays in the body for 24 hours with no major peaks. Insulins such as Levemir and Lantus are often used in conjunction with rapid-acting or short-acting insulin to help manage one’s meals throughout the day.
There is also a new treatment category for treating diabetes. GLP-1 receptor agonists only need to be injected once weekly. Medications such as Ozempic, Trulicity, Victoza, Byetta and Rybelsu have all hit the market recently.
How Diabetes medications work
These medications work similarly: They stimulate insulin release only when blood sugars climb after meals. They also suppress glucagon output by the pancreas, which decreases glucose release by the liver. The GLP-1 medications also all have a weight loss component to them. These injectables help to reduce appetite signals in the brain. By getting to a more manageable weight, one’s signs and symptoms of diabetes mellitus can often also be reduced.
As always, all the information in this article is informative only, and is not to be taken as medical advice. Please see your medical doctor for formal advice.
Barry Schustermann
Follow me on X @BarrySchust
Follow me on Facebook @ Barry Schustermann