Our immune system is profoundly impacted by high blood sugar levels and it’s functionality. Sugar triggers the release of inflammatory cytokines that systematically damage immune cells and weaken pathogen defense mechanisms. Understanding this complex process is fundamental to preventative healthcare and long-term metabolic wellness. It reveals the delicate balance between nutritional intake and cellular immunity.
Contents
Blood Sugar’s Systemic Influence
The prevalence of blood sugar disorders in the United States is staggering. Over ten percent of the population struggles with type 2 diabetes, while an additional thirty-four percent exhibit prediabetic conditions. These glucose metabolism challenges generate substantial economic and health consequences that extend far beyond individual medical experiences. The financial burden includes direct medical costs, and hospital expenses. This can create significant productivity losses at work such as absenteeism as well as presenteeism (time at work impaired due to illness).

Compromised immune responses manifest through multiple physiological pathways. People experiencing blood sugar level disruptions frequently encounter increased susceptibility to respiratory tract infections, including influenza and pneumonia. Urinary and skin infections also become more prevalent, demonstrating the comprehensive impact of metabolic imbalances on immune system resilience. The cascading effect of these disruptors can lead to chronic health challenges that extend well beyond immediate infectious risks. See Osprey Lifestyle gear for hiking, biking and travel.
The microbiome plays a critical role in this intricate biological ecosystem. Sugar consumption dramatically alters gut bacterial populations, creating significant imbalances that influence neurotransmitter production. These changes directly affect mood, anxiety levels, and cognitive function while simultaneously compromising immune response capabilities. The gut’s delicate bacterial balance becomes a critical indicator of overall metabolic and immunological health, highlighting the interconnectedness of bodily systems. Learn more about Ritual Multi Vegan Supplements.
Cellular Immunity Mechanism
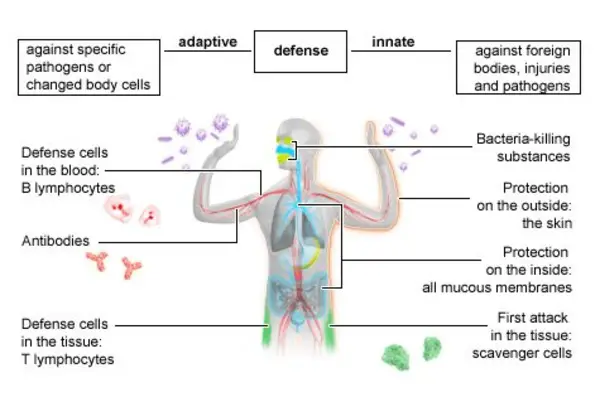
Cellular immunity mechanisms operate through two primary systems: innate and adaptive immunity. Innate immunity provides rapid responses through physical barriers like skin and mucous membranes. If pathogens pass these barriers, innate immune cells like macrophages and neutrophils engulf and destroy them. Lymphocytes, specialized white blood cells, continuously patrol the body identifying potential threats including bacteria, viruses, toxins and fungi.
Metabolic Stress and Inflammation
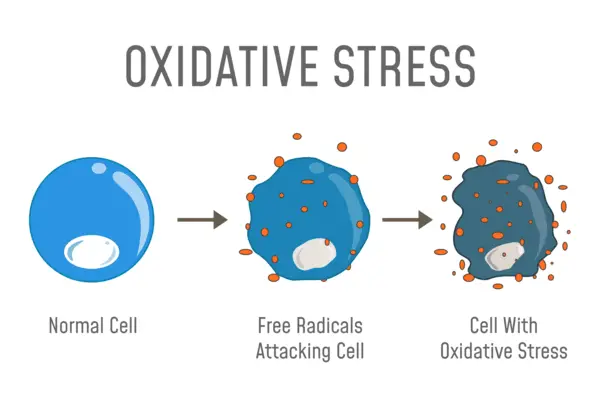
The adaptive immune system offers more targeted, long-lasting protection by developing specific antibody responses, creating a sophisticated defense. Sugar affects this aspect of the immune system the most. Metabolic stress generated by consistent high sugar intake creates substantial cellular damage. Oxidative stress weakens immune cell functionality, impairing the body’s natural defensive mechanisms. B cells’ antibody production becomes compromised, while T cells’ ability to coordinate immune responses diminishes significantly. This systematic breakdown increases vulnerability and creates a complex web of physiological interactions that undermine overall wellness. Transform your Health with Ora Organic.
The Glucose to Lymphocyte Ratio (GLR) emerges as a innovative diagnostic tool for understanding these complex interactions. This blood lab combines blood glucose levels with lymphocyte counts, potentially revealing underlying inflammation markers. Elevated GLR might indicate increased risks for heart disease, cancer and chronic infections.
Immune System Resilience
Maintaining optimal blood sugar levels represents a fundamental strategy for preserving immune system functionality. Dietary interventions, including consuming antioxidant-rich foods, managing glucose metabolism and ensuring adequate sleep can help enhance pathogen defense mechanisms.
Diagnostic Insights and Prevention
Dietary choices rich in fruits, vegetables and whole grains help support cellular immunity and reduces inflammatory markers as well as glucose metabolism. They also promote overall metabolic wellness. By understanding the relationship between blood sugar levels and immune system performance, individuals can make informed decisions about their health. One can potentially mitigate long-term health risks through proactive nutritional management.
Consultation with healthcare professionals remains essential for personalized guidance. As always, all the information in this article is informative in nature, and is not to be taken as medical advice. Please see your medical doctor or healthcare provider for formal advice.
Barry Schustermann
Follow me on X @BarrySchust
Follow me on Facebook @Barry Schustermann
On Bluesky @BarrySchust
External References:
- The impact of high blood sugar on the immune system
https://pubmed.ncbi.nlm.nih.gov/32395846/ - Prevalence of diabetes and prediabetes in the United States
https://www.ncbi.nlm.nih.gov/books/NBK279051/ - Effects of sugar on immune cell metabolism and function
https://www.mdpi.com/2673-4540/4/1/5 - Glucose metabolism reprogramming and immune escape in cancer cells:
https://www.explorationpub.com/Journals/etat/Article/1002149 - Impact of Type 2 Diabetes Mellitus on organ metabolism and the immune system
https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.01582/full